|
Friday, December 12, 2014
 Foulston Law Office is investigating and filing cases nationwide on behalf of persons who have suffered a bleeding event while on the drug Xarelto. Xarelto is a blood thinning drug manufactured and marketed through a joint venture between Bayer and Janssen Pharmaceuticals (Johnson and Johnson subsidiary). The drug was introduced to compete with the most popular blood thinner on the market Warfarin (a/k/a "Coumadin"). Xarelto is often prescribed to patients that suffer from the heart condition Atrial Fibrillation ("A-Fib") to reduce the risks of developing a blood clotting event such as a stroke. In other instances, the drug is prescribed to patients who have suffered from deep vein thrombosis ("DVT") or pulmonary embolism ("PE") for prevention of a recurrence. It is also used post-operatively in patients undergoing major surgeries of the hip, knee or pelvis commonly associated with high risk of DVT or PE. The main benefit advertised by the developers of Xarelto is that, unlike its competitor Warfarin, Xarelto does not require periodic blood-work monitoring. For example, patients on Warfarin have their clotting abilities monitored through routine blood tests. These tests are a proactive effort to achieve an appropriate therapeutic level of the drug, and to catch a sudden change in clotting abilities before dangerous clots form or drug-induced bleeds occur. Xarelto's makers claim blood-work monitoring is not required for their drug -- which is referred to in their marketing materials as the "Xarelto Difference." Not only is monitoring possible with Xarelto but critical because no antidote exists to reverse the drug’s effects. Unlike Warfarin, which can be reversed with Vitamin K, there is no way to reverse the effects of Xarelto during a bleeding event or emergency. The developers of Xarelto fail to adequately disclose this important information. A patient experiencing a Xarelto bleeding event will not respond to Vitamin K treatment. A Xarelto victim's only options are typically unsuccessful blood transfusions or dialysis procedures or to simply wait it out until the Xarelto leaves the system. Many patients do not have that kind of time. After Xarelto's first year of promotion and sales, the "reported" adverse events to the FDA had nearly triple the number of deaths than that of Warfarin in the same year. As a result of the lack of development toward an antidote and routine blood-work monitoring guidelines, these adverse events and tragedies are and will remain the reality for Xarelto consumers. The Foulston Law Office believes that the failure to monitor a drug with a known risk of bleeding and selling a drug without an antidote to stop a bleeding event is extremely reckless. We are taking cases for any patient on Xarelto who was hospitalized for any period of time due to a bleeding event or cases involving a death caused by uncontrolled bleeding. For further information please call our office.
Monday, November 10, 2014
 Talcum powder has been found to cause ovarian cancer when used by women for perineal hygiene. Johnson & Johnson, a major manufacturer of talc-based baby powder and body powder, has been accused of failing to warn consumers of the risks of talcum powder. As many as 10,000 women develop ovarian cancer each year as a result of baby powder use, says Harvard epidemiologist Dr. Daniel Cramer. Ovarian cancer is a serious disease and is expected to result in more than 14,000 deaths this year in the United States. In October of 2013, a federal jury found manufacturer Johnson & Johnson at fault in the case of a South Dakota woman who developed ovarian cancer after having used the talcum-based product regularly for thirty years. The company’s attorney claimed that while it had known for years of its product's propensity for causing cancer, it felt the risk too small to warrant a warning to the public. Research suggests that talc-based products used for feminine hygiene purposes can lead to an increased risk of developing ovarian cancer. Unfortunately, ovarian cancer doesn't always manifest until the disease is spread beyond the ovaries. It is estimated that only 20% of women receive an early diagnosis, when the cancer is most easily cured. Early detection of ovarian cancer is paramount, considering the 5-year survival rate for all cases is a mere 40%. Talcum powder is made from talc, a mineral made up mainly of the elements magnesium, silicon, and oxygen. As a powder, it absorbs moisture well and helps cut down on friction, making it useful for keeping skin dry and helping to prevent rashes. It is widely used in cosmetic products such as baby powder and adult body and facial powders, as well as in a number of other consumer products. As early as the 1970's medical researchers in the field of ovarian cancer detected talc fibers in the ovarian tissues of women diagnosed with cancer. In 2003, a meta-analysis examining 16 previous talcum powder ovarian cancer research was published confirming that weekly use of baby powder increases the risk of ovarian cancer by 33%. How do I know if my ovarian cancer was caused by talcum powder? By reviewing your medical records and sending your pathology reports to a talcum powder ovarian cancer expert, we can help determine whether talc may have caused your ovarian cancer. Talc fibers can be found in the ovaries, Fallopian tubes and in the pelvic lymph nodes for years after entering the female reproductive system. If talc fibers are present in your ovarian tissues, our researchers will detect them. Individual who have used talcum powder or talc-based baby powderon a regular basis in the past are most likely to develop ovarian cancer. Ovarian cancer symptoms: - include pelvic pain, pressure and discomfort:
- abnormal bleeding
- bloating
- constant fatigue
- sudden weight loss or weight gain
- feeling sated quickly or difficulty eating
- frequent urination
- Constipation
- Shortness of breath
- Pain during intercourse
- Nausea and indigestion
- Back pain.
Contact the law office of Steven L. Foulston to obtain further information to assist you.
Tuesday, October 21, 2014
Law360, New York (October 17, 2014, 6:13 PM ET) -- The first trial in West Virginia state court over allegations that Takeda Pharmaceutical Co. Ltd.'s widely prescribed diabetes drug Actos causes bladder cancer begins Monday, featuring the same plaintiffs firm that has taken Actos cases to trial in four other states and secured three pro-plaintiff verdicts.
Read more . . .
Tuesday, July 29, 2014
JULY 28, 2014By: Jacky Gale Judge Carol E. Higbee upheld an $11.1 million jury verdict, which resolved a vaginal mesh lawsuit filed in 2008 on behalf of a woman and her husband. Johnson & Johnson and the company’s subsidiary, Ethicon, had sought to overturn the verdict. However, Judge Higbee rejected the company’s post-trial motions and denied their request for a new trial. The vaginal mesh lawsuit verdict awarded the plaintiff $3.35 million in compensatory damages, plus $7.76 million in punitive damages. According to the plaintiff’s complaint, she had received the defendant’s Gynecare Prolift sling device during a surgery in 2006 for the purpose of treating pelvic organ prolapse (POP). Her lawsuit claimed the device hardened improperly while it was inside her and subsequently eroded through the vaginal wall. Her lawsuit pointed to 18 subsequent surgeries she was forced to undergo, which removed pieces of the mesh. Despite the revision surgeries, the plaintiff alleged significant and unresolvable pain that interfered with her ability to sit and caused intercourse to be painful. Vaginal mesh lawsuit verdict upheld for Gynecare plaintiff The plaintiff received the favorable verdict in February 2013, after which Johnson & Johnson attempted to appeal. The defendants claimed in their post-trial motions that the punitive damages were not allowable by the law and that the plaintiff’s evidence did not adequately prove her claims. Ethicon further argued that the jury verdict involved an excessive amount of money. Judge Higbee rejected the defendants’ arguments, stating that the evidence presented at trial was sufficient to support the plaintiff’s claim that Ethicon had withheld warnings of the risks of the Gynecare mesh, despite knowing that there were problems with it. Johnson & Johnson had attempted to argue that punitive damages were erroneously awarded because, under New Jersey law, the FDA’s approval preempted them. However, as the Judge noted in her ruling, the plaintiff’s injuries were sustained two years before the FDA granted approval for the medical device. Therefore, the Judge ruled the plaintiff could be granted punitive damages. Judge Higbee further noted that the substantial size of the vaginal mesh lawsuit verdict was not excessive because the jury could have granted even more in damages. Gynecare mesh withdrawn from the market On May 10, 2012, Ethicon informed the FDA that it planned to withdraw many of its Gynecare mesh products from the market. This move did not constitute a recall of the device. The company still planned to continue selling its Gynecare Gynemesh product, with the caveat that it be inserted only through the abdomen, rather than the vagina. The defendants planned to withdraw the products gradually, phasing them out completely by the beginning of 2013. Industry experts speculated that the withdrawal of the products from the market was in response to the numerous adverse event reports involving serious complications, in addition to several deaths reportedly associated with the devices. Additionally, while the plaintiff in this particular vaginal mesh lawsuit has achieved resolution of her case, Johnson & Johnson still faces thousands of product liability lawsuits filed by plaintiffs who received the product. To date, there are still over 18,000 lawsuits pending against Johnson & Johnson, with a total of almost 60,000 lawsuits filed against manufacturers who designed and sold similar vaginal mesh devices. The federal cases have been consolidated as part of various transvaginal multidistrict litigation [MDL]
Wednesday, June 25, 2014
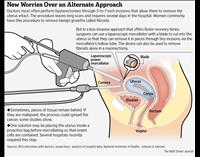
Medical Device May Spread Cancer
- During your fibroid surgery or hysterectomy your doctor may have inadvertently spread a hidden cancer throughout your body. Many women have hidden cancers in the uterus which cannot be determined until after surgery.
- The Food and Drug Administration (FDA) points out that a popular medical tool used in laparoscopic surgeries, the power morcellator, has spinning blades that cut out tissue. When this happens, they can accidentally stir up tumorcells, and your cancer can move into other organs.
- Although the FDA discourages doctors from using power morcellators and asks them to warn patients of this possibility, the device has not been recalled yet.
- Many patients suffer from this problem because power morcellator procedures are thought to provide shorter hospital stays, lower infection rates, and quicker procedures. This is due to the small incision and shorter recovery time than a typical surgery requires.
- And since it is difficult to diagnose cancer before surgery, the doctors are unaware that they are spraying dangerous tissue throughout your body cavity.
- This speeds up the progression of your illness. The faster the cancer spreads and the more virulent it becomes, the more likely you are to die sooner.
- Power morcellators are also used for renal and spleen surgery, and you can end up with tumors growing on other organs in these situations also.
Do Power Morcellators Spread Anything Besides Cancer?
- Unfortunately, yes. In some cases, power morcellators can also spread uterine and fibroid tissue to other abdominal organs. This can cause infections or bowel obstruction. You may need additional surgery to remove these growths.
Ethicon / Johnson & Johnson Devices:
- Gynecare Morcellex
- Morcellex Sigma
- Gynecare X-Tract
- Diva
Foulston Law is sensitive to the tragic consequences of surgeries performed with power morcellators. Thousands of women have been put at risk by the companies who made these devices, and Foulston Law is here to help.
Monday, April 28, 2014
 The Courtroom Controversy Behind Popular Contraceptive Mirena
By Victoria Bekiempis / April 24, 2014 1:04 PM EDT
K. was in the shower when she realized something was wrong. She was shampooing her long, red-brown tresses when suddenly, clump after clump tumbled toward the drain. She might have dismissed this as an anomaly—after all, she had given birth to a baby boy six months earlier, and postpartum hair loss, while rare, was nonetheless a possibility—but she had been given a clean bill of health after pregnancy, and had also noticed other problems. She gained 50 pounds; she felt unrelenting fatigue; intercourse became so painful that she recoiled from her husband’s touch; she grew so tired and moody that doctors thought she was depressed or bipolar.
Aside from the baby, K. could think of only one thing that was different in her life: A few months after giving birth, K.’s doctor inserted Mirena, an increasingly popular hormonal intrauterine device that can prevent pregnancy for up to five years. K. demanded her gynecologist remove the device but the doctor couldn’t find it, so she had to have surgery. The Mirena had perforated K.’s uterus and migrated into the abdomen until lodging in her omentum, tissue that protects and connects the internal organs.
Removing the IUD didn’t fix things: Scar tissue related to migration grew, resulting in painful cysts and blocking organs. She has since had four more surgeries to remove scar tissue, including a hysterectomy at the age of 24 that left her infertile. Last week, K. learned she will need another procedure, as the scar tissue keeps returning.
She is one of more than 1,200 women nationwide claiming side effects, including perforation, migration, pelvic inflammatory disease, ectopic pregnancy and, in the most extreme cases like K.’s, painful surgeries and even hysterectomy. Many have filed lawsuits against Bayer, which makes Mirena, and the cases are moving toward class-action status.
And yet K.’s story is exceedingly unusual from a medical standpoint. Approximately 2 million women across the country, and millions more worldwide, use Mirena, and the overwhelming majority have done so for years without incident. The risk of adverse effects like K.’s is approximately one in a thousand, which clinicians, the Food and Drug Administration (FDA) and, of course, Bayer, have agreed is an acceptable rate and comparable to other forms of birth control.
Many plaintiffs’ lawyers aren’t arguing that Mirena is flawed per se; instead, they’re saying Bayer should have done more to warn patients about worst-case-scenario side effects, rather than just mentioning it in the full prescribing information. Bayer rejects that.
“Based on the totality of data available to date, a positive benefit-risk profile continues to be observed with Mirena,” Bayer wrote in a statement to Newsweek. “Bayer has adequately disclosed all known risks associated with Mirena since the FDA first approved it in 2000. Any allegation that Bayer failed to adequately warn of these risks is not based in fact.”
The company’s lawyers recently asked a judge to dismiss many of the cases, claiming they were filed so long after the alleged injuries that they shouldn’t be heard.
The FDA has come down on Bayer for Mirena marketing tactics in one instance, specifically for minimizing risks.
In 2009, Bayer partnered with a social networking site called Mom Central to organize in-home IUD marketing events. A Bayer representative touted the romantic benefits of Mirena at these parties. The FDA said this program violated pharmaceutical marketing regulations, writing in a letter to the company that these claims “misleadingly overstate” Mirena’s efficacy and that the rest of the presentation failed to disclose the product’s risk.
Bayer downplays the Mom Central incident: There were only three gatherings attended by a total of 80 people, and the program was promptly discontinued, the company says.
Many users and medical professionals consider Mirena, along with its chief rival, the copper-containing ParaGard, to be the best birth control available.New York magazine reported that users, who make up 5.6 percent of birth control users today, like these products so much that there’s an “IUD evangelism” trend—women are satisfied to the point where they enthusiastically spread the word about the product to friends, family and, really, anyone who’ll listen.
This is a dramatic shift in public opinion toward the IUD, which first went on sale in the U.S. in the 1960s. Though most of the early IUDs were safe and effective, a flawed model called the Dalkon Shield caused so many pelvic infections, some of which led to hysterectomies and at least 18 deaths, that the makers pulled it from the market in 1974. Lawsuits led to some 200,000 settlements and a $3 billion trust for victims. The bad press toward the Dalkon Shield, while justified, wound up turning women away from all IUDs.
Family planning experts did not abandon the idea behind the IUD, and new models were developed, such as the ParaGard (approved by the FDA in 1984) and, later, Mirena, which have gradually reduced the stigma caused by the Dalkon Shield.
There are several reasons for this. “The failure rate is somewhere around 0.2 percent, compared to 5 to 7 percent with the pill,” and the side effects are minimal, says Dr. Petra Casey, associate professor of obstetrics and gynecology and director of the Mayo Clinic’s Contraception Practice in Rochester, Minn. “It should be considered a first-line contraceptive.”
The risk of severe side effects with Mirena is about the same as that for oral birth control pills. It’s not a perfect comparison, since the two methods have different kinds of severe side effects. But the most-feared risk with the pill, blood clots, is reported at a rate of approximately 1 to 3 women per 1,000, which, again, is around that of Mirena.
Dr. Anne Burke, an assistant professor of gynecology and obstetrics at the Johns Hopkins University School of Medicine, speaking on IUDs generally and not the litigation, says, “The overwhelming amount of data indicate that while these complications can happen, fortunately they’re rare. Most the women who use this device are able to use it safely.”
Women’s health experts also attest to noncontraceptive benefits of Mirena, such as Dr. Lynne Bartholomew Goltra, an ob-gyn at Massachusetts General Hospital.
“In addition to making women’s periods lighter and less painful, it may lessen the pain from endometriosis and may prevent some pelvic infections [pelvic inflammatory disease],” Goltra says. “It has been used to prevent the development of precancerous endometrial hyperplasia in women at higher risk of developing this and is effective in treating some types of this condition.”
Women’s health professionals have encouraged greater use of IUDs because they are more reliable than other methods and therefore prevent many more unintended pregnancies. Pregnancy is in itself a condition that carries risk, with complications ranging from ectopic pregnancy to pre-eclampsia, diabetes and urinary tract infections. Unintended pregnancies can be even more risky if the mother has not taken precautions such as giving up smoking and alcohol. Among developed countries, the United States has among the highest rates of unintended pregnancies: 51 percent of the 6.6 million pregnancies nationwide.Lawyers involved with the cases argue that Mirena’s success with most woman doesn’t mean much to the the minority who have suffered.
Carmen Scott, who leads pharmaceutical litigation with Mount Pleasant, S.C.–based Motley Rice and has worked on many reproductive health cases, says that the device’s negative impact is apparent in the hundreds of women represented by her firm.
“Many of the women that this product is prescribed to are very young and plan on having families,” Scott, who’s arguing many of these Mirena cases, says.
“This device has prevented that in many young women.”
Bayer, which does indicate that perforation can happen upon insertion, needs to make clearer that perforation can take place long after the IUD is implanted, says James Ronca, an attorney at the Philadelphia-based firm Anapol Schwartz who represents many Mirena plaintiffs.
“If 500 people were on a 747 and it crashed or there were some other incident where a lot of people were injured, planes would be grounded and there would be an investigation,” Ronca says.
By extension, the 2,000 people expected to sue Bayer is not “an insignificant number” and worth an additional warning, he says.
In this complicated case, however, it’s not just Bayer whose marketing tactics have been called into question. Some of the lawyers representing plaintiffs have drawn ire for their ads from legal reformers and physicians. Many women who complain about Mirena learn of litigation via prominently displayed search engine ads or social media.
Dr. Nancy L. Stanwood, a member of the American College of Obstetricians and Gynecologists’ work group on long-term contraceptives, said that Mirena lawsuit commercials airing in her area have “scared off” women who would greatly benefit from the device.
“It’s clear that those commercials are designed to be scary and to not put the medical facts in appropriate context,” she says, which “is unfortunate and a disservice to women having a full and accurate understanding of what their contraceptive options are.”
Monday, April 21, 2014
Free samples of prescription drugs are costly to patients, study says
By Karen Kaplan
April 16, 2014, 3:42 p.m.
Free samples of prescription drugs may seem like a great deal for patients. But even when doctors think they’re doing patients a favor by handing out the freebies, the real beneficiaries are the drug manufacturers, according to new research in the journal JAMA Dermatology.
Medical groups have grown increasingly wary about free drug samples, and they've already been banned by Kaiser Permanente, many academic medical centers, the Veterans Health Administration, the US Military and plenty of private medical clinics. Critics of the practice say it encourages doctors to prescribe drugs that are more expensive and potentially less safe than the work-horse generics that are just as effective. If the goal is to make costly medications available to low-income and uninsured patients, there are better ways, they say.
Yet $6.3 billion worth of free samples were handed out to doctors in 2011, according to the market research firm Cegedim Strategic Data [as quoted]by American Medical News). Among physicians, dermatologists are particularly likely to give free samples to their patients.
A group of researchers from Stanford University took a close look at how those free samples might be influencing the prescriptions written by dermatologists. They focused on prescriptions for patients with a new diagnosis of adult acne (either acne vulgaris or rosacea).
Based on survey data from the National Disease and Therapeutic Index, the researchers found that dermatologists were still enamored with free samples. In 2010, 18% of all prescriptions they wrote came with a free sample, up from 12% in 2001. That was in marked contrast to doctors from other specialties: Only 4% of their combined prescriptions were accompanied by a free sample in 2010, down from 7% in 2001.
Dermatologists were especially likely to give free samples to their adult acne patients – 25% of their prescriptions came with a free sample in 2010, up from 10% in 2001. Very often, the drugs that were most frequently prescribed with a free sample were also the most frequently prescribed overall. In 2005, for instance, the four acne medications most often prescribed with a free sample – Differin, Duac, Benzaclin and Retin-A Micro – were the four most-prescribed acne drugs as well, the researchers found.
It’s not just that these four drugs were perennial favorites. The list of top five acne drugs changed considerably between 2001 and 2010, according to the study. But the favorites were usually closely aligned with the drugs that doctors had available for free in their offices.
In 2010, nine of the 10 most popular acne drugs nationwide were either brand-name drugs or branded generics (which companies sell at a premium), and free samples for them are typically available. To get a sense of whether things would be different in the absence of free samples, the researchers examined the prescribing behavior of dermatologists at an academic medical center that had a policy against freebies. In this group, nine of the 10 most popular acne drugs were low-cost generics (which don’t come with free samples).
Similarly, in 2010, 79% of acne prescriptions in private practices were for name-brand or branded generic drugs, compared with 17% of prescriptions written by the academic dermatologists.
“Prescribing preferences are at least in part related to what is contemporaneously available as free samples,” the Stanford researchers wrote.
It doesn’t seem that the free samples wound up saving patients much money. Those who were seen in private practices walked away with prescriptions for $465 worth of medications, on average, while the patients treated at the academic medical center got prescriptions that cost about $200 to fill. “In other words, the national mean retail cost of the prescriptions received at an office visit for acne is conservatively two times higher compared with the AMC (academic medical center), where samples were unavailable,” the researchers concluded.
In an editorial that accompanied the study, three dermatologists noted that this pattern had been documented before. A 2008 study in the journal Medical Care found that patients seeking treatment for a variety of ailments paid more out of their own pockets when they got free samples compared with patients who didn’t. But everyone pays, since “samples increase the cost of medicines for all patients by encouraging doctors to prescribe more expensive drugs,” they wrote.
The trio called on their fellow dermatologists and other physicians to steer clear of free samples: “Alongside those other inappropriate tools of drug marketing – sports tickets, Caribbean junkets, and free pens – samples belong not in dermatologists’ closets, but in our dustbins.”
Monday, April 21, 2014
 WALL STREET JOURNAL
FDA Advises Against Morcellator Use in Hysterectomies
Citing Cancer Risks, Overseer Discourages Use of Morcellators to Remove Uterine Growths
By
JON KAMP and
JENNIFER LEVITZ
Updated April 17, 2014 8:26 p.m. ET
Federal regulators advised doctors Thursday to stop using a surgical device used in tens of thousands of hysterectomies each year, citing its potential to spread cancer.
The move by the Food and Drug Administration could change the way many women are treated for common but often painful growths in the uterus known as symptomatic fibroids, which spur about 40% of the roughly half-million hysterectomies performed annually in the U.S., by some estimates.
The agency's safety alert follows a series of articles in The Wall Street Journal that reported on the risk of using the device and a campaign started earlier by two Boston-area physicians to halt the procedures.
The instrument, known as a power morcellator, typically uses a tube-shaped blade to slice up and remove fibroids or the entire uterus, avoiding the long surgical scars associated with traditional, open surgery. But it can also spread an often undetectable cancer known as a uterine sarcoma, according to the FDA.
In a rare safety alert for medical devices—addressed to doctors, medical associations, hospitals, women, device manufacturers and advocacy groups—the FDA cited estimates that this cancer affects one in 350 women undergoing such procedures and that power morcellation can significantly worsen the odds of long-term survival.
"For this reason, and because there is no reliable method for predicting whether a woman with fibroids may have a uterine sarcoma, the FDA discourages the use of laparoscopic power morcellation during hysterectomy or myomectomy for uterine fibroids," the agency said in a communication posted on its websiteThursday. Myomectomy is the removal of just fibroids.
"In general, the procedure should not be performed," Dr. William Maisel, deputy director for science and chief scientist at the FDA's Center for Devices and Radiological Health, said at a media briefing.
If doctors do perform such procedures, the FDA said, they should advise patients of the cancer-spreading risk.
The concern is that using a powered device to slice undetected, cancerous tissue within the abdomen—and without any protective measures—raises the risk of malignant cancer cells embedding in other tissue and elevating the cancer to a more dangerous stage, studies have shown.
Because uterine sarcomas can't be reliably detected before they are removed, they can be mistaken for fibroids. The cancer is typically discovered only after the mass has been removed and tissue sent to a pathologist.
Amy Reed and her husband, Hooman Noorchashm, at home in February. Gretchen Ertl for The Wall Street Journal
This was the situation that ensnared Amy Reed, a 41-year-old mother of six and anesthesiologist at Boston's Beth Israel Deaconess Medical Center, who developed advanced uterine cancer shortly after a routine hysterectomy in October. The hospital where she was treated, Boston's Brigham and Women's Hospital, acknowledged that use of morcellation worsened her cancer.
The FDA began its review in December, "when some high-profile cases covered in the media came to our attention," Dr. Maisel said. The agency also noted there are many alternatives, including minimally invasive surgery without morcellators, vaginal hysterectomies and open surgery. There are also nonsurgical options including drug therapy and ultrasound treatment.
The agency's alert prompted some to act immediately Thursday. Dr. Isaac Schiff, chief of the Department of Obstetrics & Gynecology at Massachusetts General Hospital, said, "I have asked our doctors to stop the procedure immediately until we have more information."
Robert Barbieri, obstetrics and gynecology chairman at Brigham and Women's Hospital, told surgeons Thursday that "we are immediately suspending use of this device in all cases until further notice," according to an emailed statement. Both hospitals had previously put tight restrictions on morcellators in response to cancer concerns.
Morcellators, introduced in the 1990s, have helped gynecologists perform about 50,000 fibroid-removal procedures each year through tiny holes, the FDA estimated, rather than longer incisions that can lead to bigger scars and a longer recovery.
The FDA doesn't directly regulate how doctors practice medicine, but advising against a procedure can significantly change practice by raising the risk of lawsuits for doctors who go against that advice, legal experts said.
"The fact that the FDA released this warning makes it more likely that a doctor who went against it will be held to have practiced in a way below the standard of care," said I. Glenn Cohen, a Harvard Law School professor who specializes in health-law policy and bioethics. "Second, this increases the chance that a patient may succeed in suing for a failure to get informed consent."
"Doctors have to act within a standard of care," Robert J. Gordon, a partner at law firm Weitz & Luxenberg in New York. "What the FDA says about a procedure goes a long way to establishing what the standard of care is for a jury."
Dr. Maisel said the clinical community has been aware of the risk of cancer since the advent of the procedure, although he said the rate of that risk is only now coming into focus. He also said it is conceivable that some patients may believe the risks of alternative procedures outweigh the risks of laparoscopic surgery with morcellation. They should be explicitly told of the risks, he said.
With the issue gathering steam since December, gynecological societies had already been doing their own reviews of power morcellation. Commenting on the FDA move, the American College of Obstetricians and Gynecologists said its own review, which includes an assessment of risks for various groups of patients, is ongoing. "We greatly appreciate the urgency behind the issue," the group said.
Dr. Maisel said older women have a higher risk of having a hidden sarcoma than younger women.
Some gynecologist have argued there are several ways to perform minimally invasive procedures without using morcellators, including cutting tissue manually inside protective bags. Gynecologists have said they seldom used these bags during hysterectomies and fibroid procedures previously.
A number of top hospitals have recently told their doctors only to morcellate inside bags. The FDA said it would convene a public advisory committee meeting this summer to discuss whether such bags can enhance the effective use of morcellators, amid other issues. The FDA instructed morcellator manufacturers "to review their current product labeling for accurate risk information for patients and providers."
The FDA noted these changes, although Dr. Maisel also said bags have some downside, including obscuring surgeons' view during procedures, and are "not a panacea."
A spokesman for Johnson & Johnson's Ethicon subsidiary, the largest maker of power morcellators, said the company will review its product labeling as the FDA requested and supports plans for an advisory committee meeting. He noted that J&J's uterine morcellator instructions have always recommended doctors use protective bags when using the device on malignant or suspicious tissue.
"This is an important announcement by the FDA, and we support any measures that enhance patient safety, which is always our first priority," the spokesman said.
The FDA recommended "routine follow-up" with physicians for women who have already had hysterectomies or myomectomies, don't have symptoms and were told postsurgery tests were normal. Tissue is commonly checked for cancer afterward. But women with "persistent or recurrent symptoms or questions should consult their health-care provider," the agency said.
Diana Zuckerman, president of the nonprofit National Research Center for Women & Families, and an advocate for stiffer medical-device regulations, said the FDA's statement should have a major impact. "What surgeon is going to take the chance of using this device if the FDA has made such a strong warning?" she said. The FDA's action "is going to save a lot of lives."
Tuesday, April 8, 2014
Bloomberg News
By Jeff Feeley April 04, 2014
Johnson & Johnson was ordered by a Texas jury to pay $1.2 million to a woman who alleged one of the company’s lines of vaginal-mesh implants to treat incontinence was defectively designed, in the first verdict against the company over those devices.
Jurors in state court in Dallas concluded the design of the TVT-O mesh sling implanted in Linda Batiste was flawed and the 64-year-old woman deserved $1.2 million in compensatory damages, her lawyers said. They argued Batiste suffered pelvic pain when the device eroded inside her.
J&J, based in New Brunswick, New Jersey, faces more than 12,000 lawsuits accusing its Ethicon unit of making improperly designed vaginal inserts, such as the slings, that damaged women’s organs and made sex painful. Most of the cases have been consolidated before a federal judge in West Virginia for pretrial information exchanges while other cases are being heard in state courts.
The U.S. Food and Drug Administration has ordered J&J, C.R. Bard Inc. and 31 other vaginal-implant makers to study rates of organ damage and complications linked to the implants after manufacturers faced a wave of lawsuits over the devices.
Doctors inserted more than 70,000 mesh devices in the U.S. in 2010 alone, threading them through incisions in the vagina to fortify pelvic muscles that failed to support internal organs or to treat incontinence, according to court filings.
Appeal Planned
J&J officials noted the Dallas jury rejected Batiste’s claims that Ethicon didn’t provide proper warnings about the slings’ health risks and declined to award punitive damages.
“The jury’s verdict on design defect is disappointing, and we believe we have strong grounds for appeal,” Matthew Johnson, an Ethicon spokesman, said yesterday in an e-mailed statement.
J&J officials decided in 2012 to stop selling some lines of vaginal-mesh implants after being hit with a wave of lawsuits over the devices. The TVT-O sling Batiste, a former nurse, received is still on the market, Thomas Cartmell, one of her lawyers, said in a phone interview.
“This verdict represents the first time an impartial jury had the opportunity to decide whether Ethicon’s sling products are defective and they found exactly that,” Bryan Aylstock, a plaintiffs’ lawyer helping to oversee cases gathered before U.S. District Judge Joseph Goodwin in West Virginia, said in a phone interview. “We believe this is the first of many more verdicts to come over this dangerous product,” he added.
NJ Verdict
Last year, a New Jersey jury ruled J&J must pay $11.1 million in damages to a woman who blamed a Prolift device for her injuries in the first case over any of the company’s implants to go to trial. The Prolift implants help support sagging organs.
Lawyers for J&J, the world’s biggest maker of medical products, argued in court papers that the TVT-O slings are safe and effective and the company properly warned consumers about their risks.
In February, Goodwin threw out a woman’s claims that another line of the company’s sling inserts was defective.
The Texas case is Batiste v. McNabb, No. 12-14350, District Court for the 95th Judicial District, Dallas County Texas (Dallas). The West Virginia case is In Re Ethicon Pelvic Repair System Products Liability Litigation, 12-MD-02327, U.S. District Court, Southern District of West Virginia (Charleston).
Tuesday, April 8, 2014
Actos Verdict: Jury Orders Takeda, Eli Lilly To Pay $9 Billion In Damages
Reuters
Posted: 04/08/2014 12:28 am EDT Updated: 04/08/2014 10:59 am EDT
April 8 (Reuters) - A U.S. jury ordered Takeda Pharmaceutical Co Ltd to pay $6 billion in punitive damages and Eli Lilly and Co to pay $3 billion in a case claiming that cancer risks to the diabetes drug Actos were concealed, the plaintiffs' lawyer said.
The lawyer, Mark Lanier, said there was "stunned silence" in the packed courtroom following the announcement of the damages.
The jury in Lafayette, Louisiana also ordered the payment of $1.475 million in compensatory damages in the suit.
Takeda's shares in Tokyo tumbled 8.4 percent to 4,415 yen following news of the verdict.
The case number is 11-MD-2299. (Reporting by Daniel Levine in San Francisco; Writing by Edmund Klamann)
Tuesday, April 8, 2014
BY DANIEL LEVINE AND EDMUND KLAMANN
SAN FRANCISCO/TOKYO Tue Apr 8, 2014 1:36pm EDT
(Reuters) - Takeda Pharmaceutical Co Ltd said it would contest $6 billion in punitive damages imposed by a jury in the United States in a case that accused Japan's largest drugmaker of concealing cancer risks associated with its Actos diabetes drug.
Eli Lilly and Co, Takeda's co-defendant in the case, was ordered to pay $3 billion in punitive damages by the jury in Louisiana on Monday. It also awarded $1.475 million in compensatory damages.
Legal experts said it was unlikely that such a large award would stand after challenges in court by both companies. Eli Lilly and Takeda have said they would dispute the verdict, which could include appeals to a higher court or filing motions asking the trial judge to set aside or reduce the verdict.
"Although there's no mathematical bright line" to determine how high is too high when it comes to punitive damage awards, federal appeals courts generally scrutinize the ratio of punitive to compensatory damages, preferring those that fall into the single-digit range, according to Professor Catherine Sharkey, a tort law expert at New York University School of Law.
Punitive damages are meant to discourage companies from bad conduct. Compensatory damages are meant to pay victims for their actual losses. With a ratio of more than 6,100 to 1 of punitive to compensatory damages, the Actos award could be highly vulnerable.
"It's definitely the case that the U.S. Supreme Court has signaled to lower courts that they should be restraining very large punitive awards," Sharkey added.
Lilly, which co-promoted Actos from 1999 to 2006, said in a press release it will be indemnified by Takeda for its losses and expenses around the litigation based on the terms of its agreement with Takeda.
Takeda's shares fell as much as 8.8 percent to an eight-month low in Tokyo trading on Tuesday after the verdict. The stock ended 5.2 percent lower at 4,572 yen.
Lilly shares fell 0.2 percent, or 12 cents per share, to $58.50 per share in New York Stock Exchange trading.
The massive award was met with "stunned silence" in the Lafayette, Louisiana, courtroom, plaintiffs' lawyer Mark Lanier said.
Lanier acknowledged it was not certain whether the damages award would be sustained.
"Nobody has gone out and bought a new home," Lanier said.
"This is a conservative judge and a conservative court and she's very 'balls and strikes.' We're not under any grand illusion."
The $9 billion in punitive damages awarded by the jury against Takeda and Eli Lilly exceed the $5 billion penalty that a jury in Alaska imposed on Exxon Mobil Corp for the Exxon Valdez oil spill in 1989.
The U.S. Supreme Court ruled in 2008 that the previous Exxon Valdez award had been "excessive." The company was ultimately ordered to pay $500 million. That and other rulings have been read as limiting punitive damages in federal cases.
Lanier said the jury deliberated for only an hour and 10 minutes to deliver its verdict finding liability on all 14 questions, and 45 minutes longer to come out with the multibillion-dollar punitive damages.
The allocation of liability for compensatory damages was 75 percent for Takeda and 25 percent for Lilly, according to Lilly.
Takeda said judgments were entered in Takeda's favor in all three previous Actos trials, while this was the first federal case to be tried in a consolidated multidistrict litigation comprising more than 2,900 lawsuits.
Last May, a U.S. judge had nullified a separate jury verdict for $6.5 million against Takeda after ruling that the plaintiffs failed to offer any reliable evidence that Actos had caused cancer.
Germany and France suspended use of the drug, a multibillion-dollar seller, in 2011 because of concerns about a possible link to cancer.
The case is In Re: Actos Products Liability Litigation Case U.S. District Court, Western District Louisiana, No. 6:11-md-2299.
Foulston Law Office assists clients in the State of Kansas with personal injury claims, and clients nationwide with medical device and prescription drug claims.
|
|
|
|